Are Suboxone Treatment Programs Covered by TRICARE?
Does TRICARE cover Suboxone? In many cases, yes: TRICARE prescription coverage can include buprenorphine and buprenorphine plus naloxone products (like the brand name Suboxone) when they’re prescribed by an appropriate clinician and meet TRICARE coverage rules.
The practical answer is usually less about the word “Suboxone” and more about your TRICARE plan category, the drug’s formulary status, and whether prior authorization, medical necessity paperwork, or quantity limits apply.
Our resource from TriCareRehabs.com will fully answer the question: “Does TRICARE for Suboxone?”
First, it helps to visualize two lanes. One lane is the medication benefit (the pharmacy program that helps pay for the prescription).
The other lane is the treatment setting (outpatient programs or opioid treatment programs) where medication-assisted treatment may be delivered.
TRICARE can cover medication-assisted treatment in these settings, and many people receive buprenorphine based care through office-based opioid treatment with a TRICARE authorized provider.
Read on to learn more, and remember our expert staff are only a confidential phone call away for immediate support.
What Suboxone Is, and What “Covered” Really Means
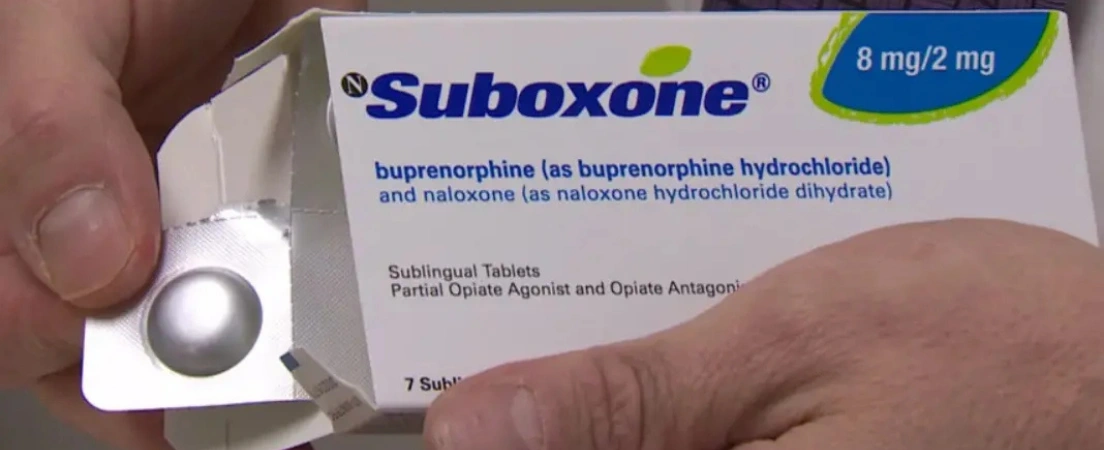
As you likely know already, Suboxone is a brand name for a combination medication that contains buprenorphine (a partial opioid agonist) and naloxone (added primarily to discourage injection misuse).
It’s used as a medication option for opioid use disorder, often as part of medication-assisted treatment (also called medications for opioid use disorder).
When people ask, “Is Suboxone covered by TRICARE?” they are usually asking one of these questions:
- Will TRICARE pay for the prescription at the pharmacy (military pharmacy, TRICARE network pharmacy, or home delivery)?
- Will TRICARE cover the doctor visits, counseling, or program where Suboxone is prescribed and monitored?
- Will TRICARE require prior authorization or a medical necessity form before the prescription is filled?
TRICARE’s pharmacy benefit is built around a formulary and coverage rules. Some medications require steps like prior authorization, medical necessity review, or adherence to quantity limits.
The Short Answer: What Does TRICARE Coverage for Suboxone Look Like?
TRICARE may cover substance use disorder treatment services that commonly wrap around Suboxone care, including higher intensity outpatient levels of care, along with medication-assisted treatment and office-based opioid treatment.
That does not mean every program is automatically covered in every circumstance, but it does mean Suboxone based treatment is not “outside the benefit” by default.
A helpful nuance is that TRICARE’s medication-assisted treatment coverage notes you don’t need pre-authorization for medication-assisted treatment, and it also notes that availability overseas can depend on host country licensing rules.
Who Can Use TRICARE for Suboxone?
In general, any TRICARE beneficiary with pharmacy coverage may be able to use TRICARE for buprenorphine based medication treatment if it’s clinically appropriate and properly prescribed.
Two common situations that change the “how” (not necessarily the “whether”) are:
- Active duty: care is often coordinated through a military treatment facility or a primary care manager, and referrals or care pathways can differ based on where you receive care.
- Family members and retirees: You may have more flexibility in where you receive office-based opioid treatment, but you still want to confirm a provider is TRICARE authorized and understand network versus non-network cost differences.
TriCareRehabs often reminds callers seeking support that a coverage question is really two questions: coverage for the medication and coverage for the care plan around it. Sorting those apart early prevents a lot of frustration later.
How TRICARE Prescription Coverage Works for Suboxone
A few points matter most for Suboxone coverage under the TRICARE pharmacy benefit:
- Generic versus brand: if a generic equivalent is available, TRICARE may require additional review for certain brand-name prescriptions.
- Prior authorization and medical necessity: Some drugs require paperwork before coverage is approved, and TRICARE directs beneficiaries to check the TRICARE Formulary to see requirements and find the right forms.
- Quantity limits: limits can differ by pharmacy type (for example, retail network fills often align with shorter supplies, while home delivery and military pharmacies can align with longer supplies), and exceptions can be possible when medical necessity is established.
Because of these moving parts, two people can both be “covered by TRICARE” and still have different experiences at the pharmacy counter depending on plan details, dosage form, and whether paperwork was needed.
What to Expect Clinically And Why Coverage Sometimes Feels Complicated?
Suboxone is typically prescribed as part of an ongoing plan that includes assessment, diagnosis, dosing that fits the stage of treatment, monitoring for cravings and withdrawal symptoms, and support for co-occurring mental health needs when present.
From an insurance perspective, what can slow things down is rarely the concept of Suboxone itself. More commonly, it is one of these bottlenecks:
- The prescription triggers a prior authorization requirement, and the form has not been submitted yet
- The prescription is written in a way that exceeds a quantity limit
- A brand product is prescribed where TRICARE expects a generic substitute or additional review
- A provider is not recognized in the way TRICARE requires for that setting, especially when care is fragmented across locations.
If you are active duty or in a safety-sensitive role, you may also have extra layers of coordination related to duty status, readiness requirements, and where care is documented. Those layers can feel personal, but they are usually administrative, not a judgment about your recovery.
TRICARE Inpatient Treatment for Suboxone
Inpatient rehab is a critical component of substance abuse treatment for individuals requiring intensive support and 24/7 medical supervision. TRICARE covers inpatient drug and alcohol rehab when it is deemed medically necessary, following specific guidelines and approval processes.
This level of care is designed for those with severe drug and alcohol addiction or co-occurring mental health conditions that require a structured, residential treatment environment. TRICARE inpatient coverage typically includes detoxification, medication-assisted treatment such as Suboxone, behavioral therapy, and comprehensive support services to help patients manage withdrawal symptoms and begin their recovery journey.
Accessing inpatient rehab under TRICARE health insurance often involves coordination with a healthcare provider to develop a treatment plan that meets the member’s health plan requirements and ensures the best possible outcomes.
Medication-Assisted Treatment And Outpatient Opioid Treatment Under TRICARE
Many people receive buprenorphine based treatment through office-based opioid addiction treatment in a clinic setting. TRICARE’s coverage overview for medication-assisted treatment describes coverage in multiple settings, including opioid treatment programs and office-based opioid treatment, and it notes provider requirements to prescribe buprenorphine.
This matters because it shapes what “a Suboxone program” looks like. Some people picture a highly structured program, while others do best with an outpatient model where medication management is integrated with therapy, psychiatry, or primary care.
What if TRICARE Does Not Cover It Right Away?
A “not covered” message at the pharmacy can mean different things:
- The medication is covered, but a prior authorization is missing
- The medication is covered, but the prescription does not match a quantity limit
- The medication is covered, but the plan expects a formulary alternative or documentation
- The medication is covered, but a specific product or strength requires a different process
TRICARE outlines how to get prior authorization or medical necessity forms and notes that approvals apply across dispensing channels once granted, depending on the type of approval.
Alternatives That May Come Up If Suboxone Is Not The Best Fit
Coverage questions sometimes arise alongside clinical questions, especially if a patient experiences side effects or the fit is not right. Depending on the situation, a clinician may discuss other medication options for opioid use disorder in different settings.
The point is not that one medication is “better,” but that opioid use disorder treatment is individualized. If you are stable on a medication that supports health and safety, the goal is often continuity, not disruption.
Get TRICARE Opioid Treatment Support Options Today
As we have broken down in great detail, TRICARE generally covers prescription drugs and medication-assisted treatment, but individual medications can have plan-specific coverage rules.
Start by confirming what your provider prescribed (brand versus generic, dose, form), then match it to formulary requirements and the setting where you are receiving care.
And if you or a loved one is suffering from an ongoing opioid abuse issue, TriCareRehabs.com offers confidential placement support at many of the leading TRICARE–approved substance abuse facilities nationwide, offering accredited support for recovery to military members and their families.
All calls are confidential, so please reach out for proven support options with us now.
FAQs Service Members And Families Ask on Suboxone and TRICARE
Does TRICARE cover Suboxone for opioid use disorder?
TRICARE can cover medication-assisted treatment and prescription drugs under its pharmacy benefit, and buprenorphine based treatment is commonly delivered through covered settings like office-based opioid treatment.
Your exact coverage depends on the formulary status of the prescribed product and whether coverage rules like prior authorization apply.
Can you use TRICARE for Suboxone if you are overseas?
TRICARE notes that the availability of medication-assisted treatment overseas can depend on host country licensing requirements. Practically, that means access can be more variable and may require extra coordination.
Are Suboxone treatment programs covered by TRICARE?
TRICARE covers substance use disorder treatment and also describes covered higher levels of outpatient care, such as intensive outpatient programs, with coverage depending on medical necessity and any applicable rules or limits.
References and Resources
- https://tricare.mil/CoveredServices/IsItCovered/MedicationAssistedTreatment
- Coast Guard Substance Abuse Program Resources - December 23, 2025
- Does TRICARE Cover Suboxone? - December 15, 2025


